Introduction
Asthma is a chronic respiratory condition affecting over 262 million people worldwide, according to the World Health Organization (WHO). Diagnosing asthma accurately is crucial to effective management and treatment. One of the most reliable methods is the pulmonary function test (PFT), which measures lung capacity, airflow, and overall respiratory function.
In this article, we’ll explore what a pulmonary function test for asthma entails, its different types, and how the results help in managing asthma symptoms effectively.
What is a Pulmonary Function Test (PFT)?
A pulmonary function test (PFT) is a non-invasive procedure that assesses how well your lungs are working. It measures lung volume, airflow, and gas exchange to determine any obstruction or restriction in breathing.
For asthma patients, PFTs help in:
Diagnosing asthma and distinguishing it from other lung diseases.
Evaluating the severity of asthma symptoms.
Monitoring how well treatment and medications are working.
Types of Pulmonary Function Tests for Asthma
There are several types of pulmonary function tests used to diagnose and monitor asthma. The most common ones include:
1. Spirometry
Spirometry is the gold standard test for asthma diagnosis. It measures the amount and speed of air a person can inhale and exhale.
How It Works: Patients take a deep breath and forcefully exhale into a spirometer, which records lung function.
Key Measurements:
Forced Vital Capacity (FVC): The total amount of air exhaled after a deep breath.
Forced Expiratory Volume (FEV1): The amount of air exhaled in the first second. Lower FEV1 values indicate airway obstruction, common in asthma.
FEV1/FVC Ratio: Helps determine the presence of airway obstruction.
Reversibility Test: If FEV1 improves after using a bronchodilator, asthma is likely the cause.
2. Peak Expiratory Flow (PEF) Test
Measures: How fast a person can exhale air.
Used for: Daily monitoring of asthma control, rather than diagnosis.
How It Works: Patients blow forcefully into a peak flow meter, and results are compared to their baseline values.
Importance: Detects narrowing of airways before symptoms appear.
3. Methacholine Challenge Test
Used for: Confirming asthma when spirometry results are unclear.
How It Works: Patients inhale increasing doses of methacholine, a substance that narrows airways. If lung function decreases significantly, asthma is likely.
Sensitivity: Can diagnose mild asthma cases that don’t always show up on standard tests.
4. FeNO (Fractional Exhaled Nitric Oxide) Test
Measures: The amount of nitric oxide in exhaled breath, an indicator of airway inflammation.
Used for: Diagnosing allergic asthma and assessing response to inhaled corticosteroids.
Benefit: Non-invasive and quick.
5. Body Plethysmography
Measures: Lung volume and airway resistance.
Used for: Distinguishing between asthma and other lung conditions like chronic obstructive pulmonary disease (COPD).
Understanding Pulmonary Function Test Results
Interpreting PFT results is crucial in asthma diagnosis. Here’s what different values indicate:
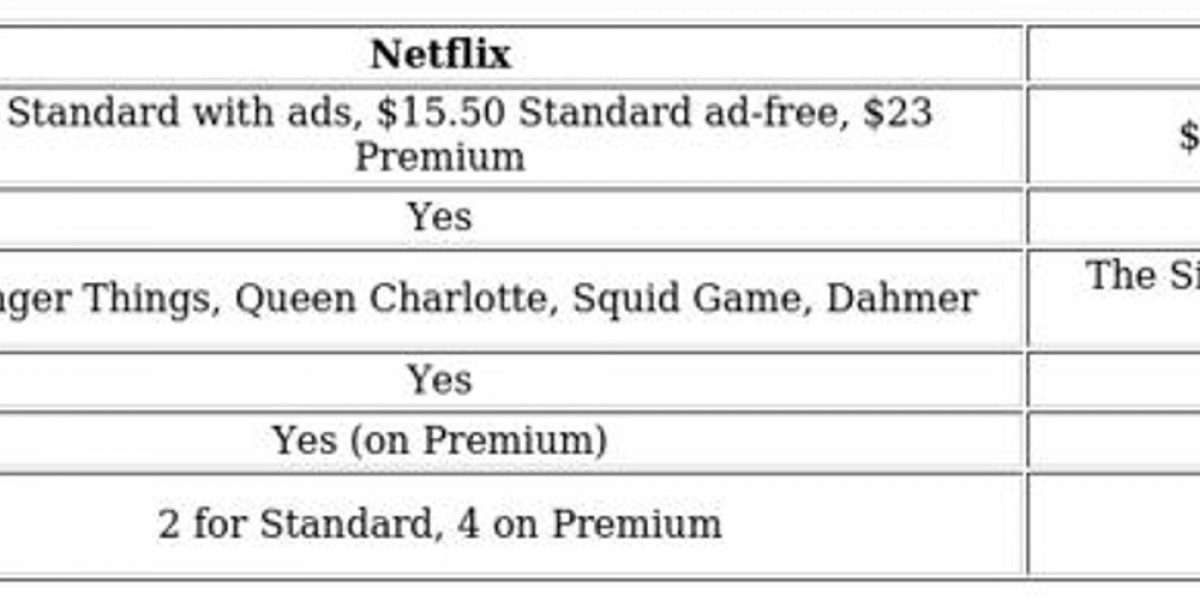
| Test Parameter | Normal Range | Asthma Indicator |
|---|---|---|
| FEV1 (Forced Expiratory Volume) | ≥80% of predicted | <80% indicates obstruction |
| FVC (Forced Vital Capacity) | ≥80% of predicted | May be reduced in severe asthma |
| FEV1/FVC Ratio | >0.7 (70%) | <0.7 indicates airflow limitation |
| Peak Expiratory Flow (PEF) | Varies by age/height | Lower values suggest obstruction |
| FeNO Levels | <25 ppb (normal) | >50 ppb suggests eosinophilic inflammation |
Asthma is confirmed if there is reversible airway obstruction (i.e., an improvement in FEV1 of at least 12% after bronchodilator use).
Who Should Get a Pulmonary Function Test for Asthma?
A PFT is recommended if you experience symptoms like:
Persistent cough, especially at night or after exercise.
Wheezing or shortness of breath.
Frequent respiratory infections.
Chest tightness.
Difficulty breathing that worsens with allergens or irritants.
When to Repeat PFTs?
During initial diagnosis.
Every 1-2 years for mild asthma.
More frequently for severe asthma or poor symptom control.
To ensure accurate results, follow these preparation steps:
Avoid smoking for at least 4 hours before the test.
Refrain from consuming caffeine as it may affect lung function.
Stop using short-acting bronchodilators 6 hours before (unless instructed otherwise).
Wear loose clothing to avoid restricting chest movement.
Inform your doctor about any medications you’re taking.
| Diagnostic Method | Purpose | Effectiveness for Asthma |
| PFT (Spirometry) | Measures lung function | Highly effective |
| Chest X-ray | Rules out other lung diseases | Not specific to asthma |
| Blood Tests | Identifies allergic triggers | Complementary test |
| Allergy Testing | Detects environmental triggers | Helps with asthma management |
| Bronchoprovocation Test | Confirms airway hyperresponsiveness | Used when spirometry is inconclusive |
Frequently Asked Questions (FAQs)
1. Is a pulmonary function test painful?
No, PFTs are non-invasive and painless. Some may experience mild discomfort from deep breathing.
2. How long does a pulmonary function test take?
Most tests take 30 to 60 minutes, depending on the type of test.
3. Can a PFT confirm asthma?
Yes, especially when there’s reversible airway obstruction shown in spirometry results.
4. How accurate are pulmonary function tests?
They are highly accurate for asthma diagnosis when conducted correctly.
5. Do I need a PFT if I already have asthma?
Yes, periodic tests help track progress and adjust treatment as needed.
Conclusion
A pulmonary function test for asthma is a critical tool for diagnosing and monitoring asthma effectively. Spirometry, FeNO tests, and peak flow monitoring help healthcare providers assess airway function and tailor treatment plans for better symptom control.
If you experience asthma symptoms, consult a doctor to schedule a pulmonary function test for an accurate diagnosis and effective treatment plan.